BONE GRAFTING AT PURE DENTAL SMILES
WHAT IS BONE GRAFTING?
Bone grafting is a straightforward operation performed by an oral surgeon. Bone grafts widen and heighten the bone around the implant site (where the implant needs to be placed.). A bone transplant is performed by attaching bone graft tissue or material to the insufficient bone region by the surgeon—collagen and proteins in the bone transplant material help promote bone development. Different types of bone transplants and surgeries for the upper and lower jaw are available.
WHAT TO EXPECT WHEN YOU NEED A BONE GRAFTING?
Following the bone grafting process, patients should expect minimal pain or discomfort. The level of discomfort is comparable to that experienced by people who have undergone other types of oral surgery or have had teeth extracted. The discomfort is usually minimal and easily controlled with over-the-counter anti-inflammatory medicine or ice bags.
Following bone graft surgery, you should expect some edema in the face. Take precautions shortly after your treatment to try to limit swelling to a minimum to decrease edema. Apply ice to the damaged parts of the face and jaw for the first two days after surgery to reduce the inflammatory process and bleeding. To sleep, prop yourself up in bed. To keep swelling under control, take anti-inflammatory drugs regularly. After Bone Graft Surgery, What to Eat

BONE GRAFTING PROCEDURE
Before the Bone grafting procedure, we will determine which sort of bone graft to utilize. You’ll be put under general anesthesia, which will put you to sleep for the duration of the procedure. An anesthesiologist will monitor the anesthetic and your recovery.
Above the area where the graft is needed, the surgeon will create an incision in the skin. The donated bone will then be shaped to fit the region. Any following will be used to keep the graft in place: pins, plates, screws, wires, cables. The surgeon will cover the incision or wound with stitches and bandage the wound once the graft is securely in place. A cast or splint may support the bone while it heals. Many times, no casting or splint is necessary.
TYPES OF BONE GRAFTING
Autograft
The use of bone sourced from the same person receiving the graft is known as autologous or autogenous bone grafting. Insignificant bones, such as the iliac crest, mandibular symphysis (chin area), and anterior mandibular ramus, can be harvested for bone (coronoid process). Autogenous bone is favored when doing a block transplant since it has a lower chance of graft rejection because it comes from the patient’s body. [3] It would be osteoconductive, as well as osteoinductive and osteogenic. The disadvantage of autologous grafts is that they require an additional surgical site, which increases the risk of postoperative pain and complications.
Allografts
Allograft is a human-derived tissue. The distinction is that allograft is taken from someone other than the person who will receive the graft. Allograft bone is obtained from cadavers who have donated their bone for living individuals in need; it is usually obtained through a bone bank.
Sterilization and deactivation of proteins contained in healthy bone are frequently required when using allografts for bone regeneration. The whole cocktail of bone growth factors, proteins, and other bioactive materials necessary for osteoinduction and successful bone healing is contained in the extracellular matrix of bone tissue; the desired characteristics and proteins are extracted from the mineralized tissue using demineralizing means such as hydrochloric acid. The mineral composition of the bone deteriorates, and the osteoinductive agents persist in a demineralized bone matrix (DBM).
Synthetic variants
The mineral to organic matrix ratio of this flexible hydrogel-hydroxyapatite (HA) composite is similar to that of normal bone. These materials are combined with growth stimulants, ions like strontium, or bone marrow aspirate to boost biological activity. Higher bone mineral density (BMD) and increased osteoblast proliferation can be achieved when components like strontium are present.
Polymer-based bone graft substitutes
Natural polymers and synthetic polymers are two types of polymers. The following are examples of polymer-based bone transplant substitutes:
- Healos is a natural polymer-based product that is a polymer-ceramic composite made up of collagen fibers that have been coated with hydroxyapatite and used for spinal fusions. It is subdivided into biodegradable and nonbiodegradable categories.
- Cortoss is a resin-based injectable solution having uses in load-bearing areas.
Xenograft
Bone grafts from animals other than humans, such as bovine, are employed as a calcified matrix in xenografts.
Alloplastic grafts
Bioactive glass or hydroxyapatite, a naturally occurring mineral (a primary mineral component of bone), can be used to make alloplastic grafts. Hydroxyapatite is the most commonly utilized synthetic bone graft because of its osteoconduction, hardness, and acceptability by bone. However, it is becoming less popular because it is entirely resorbable in a short period and makes bone-breaking easier. Calcium carbonate is used in some synthetic bone grafts. Finally, tricalcium phosphate is employed in conjunction with hydroxyapatite to provide both osteoconduction and resorbability.
Growth factors
The factors and proteins found in bone are in charge of controlling cellular activity. Growth factors attach to cell surface receptors and cause the intracellular environment to react. In general, this activity translates to a protein kinase that triggers a cascade of processes that culminate in the transcription of messenger ribonucleic acid (mRNA) and the synthesis of a protein for intracellular or extracellular function. The controlled formation and resorption of bone are the consequence of various processes’ interaction and simultaneous activity. TGF-beta, insulin-like growth factors I and II, PDGF, FGF, and BMPs are some of the characteristics found in the extracellular matrix of bone. TGF-beta, BMP-2, BMP-4, and BMP-7, when added to the culture conditions, can induce stem cells to take on an osteogenic lineage. Mesenchymal stem cells have also been sown onto bioactive ceramics that have been conditioned to stimulate osteoblast development.
Ceramic-based bone graft substitutes
Ceramics are used in most bone transplants, either alone or with other materials (e.g., calcium sulfate, bioactive glass, and calcium phosphate). Ceramics, like calcium phosphates, include calcium hydroxyapatite, which is osteoconductive, osteointegration, and osteoinductive in some situations. They have brittle characteristics and require high temperatures to produce scaffolds.
IMPLANTS BEFORE AND AFTER
BONE GRAFTING BENEFITS
Restoration
Oral surgeons can use one graft to help patients avoid additional dental and orthodontic operations by restoring bone mass and other oral tissues.
Cosmetic
Bone grafting is a procedure that supports various facial bones and structures to improve a patient’s overall appearance. As a result, a patient’s self-esteem and confidence may improve.
Improve the Use of Dental Appliances
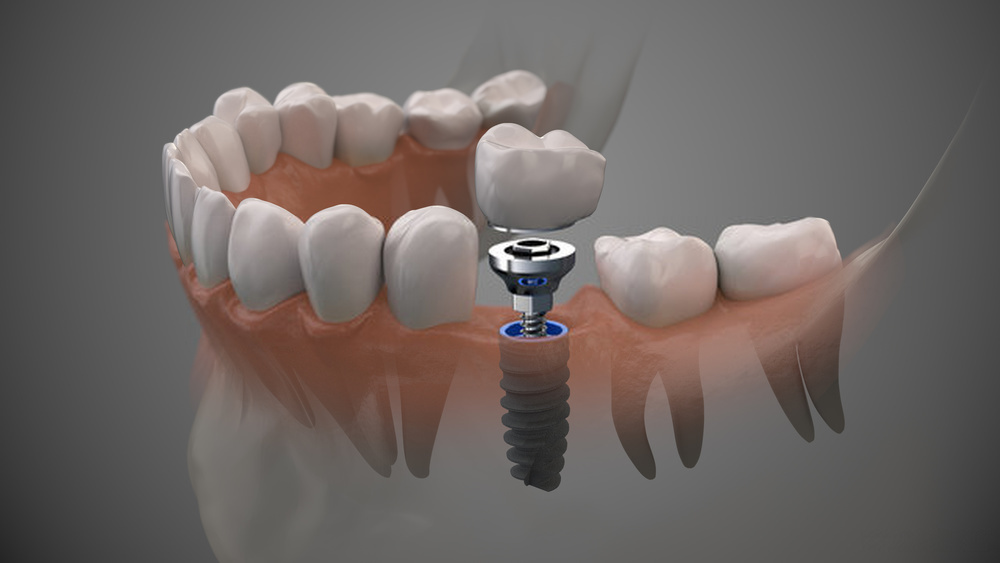
Other dental items, like crowns, implants, dentures, and bridges can be supported by bone grafts. In the long run, this will increase the function of each dental appliance.
CONTACT US TODAY
FILL OUT THE FORM BELOW AND WE’LL GET BACK TO YOU TO SCHEDULE AN APPOINTMENT.
FQA
Your recovery could take anywhere from two to three months, but the bone graft will take three months to heal. However, you will be urged to refrain from performing strenuous exercises for at least six months and keep the bone graft region clean and dry.
You may resume brushing and flossing all teeth except the surgical area 24 hours after surgery.
In general, recovery time can range from two weeks to more than two months. If a patient needs dental implants, they must wait until the bone graft has fused with the existing bone structure in the mouth. It ordinarily takes a few months for this to happen.
Most individuals with bone grafts are pain-free and do well as long as they take their medicines. In addition, your dentist must wait for the bone graft to bond with the existing bones in your mouth.
Following are some suggestions for after-surgery care for your socket bone graft: 2 hours of the firm, moist Gauze pressure: The bleeding is stopped by applying firm, moist gauze pressure. Bite down hard and keep your mouth shut during this period. Relax while watching TV while sitting upright in a comfortable chair.
In general, after a few weeks, you should feel more normal. Your bone graft will need time to mend and generate a new jawbone after your first recuperation.

